
Anemia: Common Causes, Symptoms, Types, and Treatment
What Is Anemia?
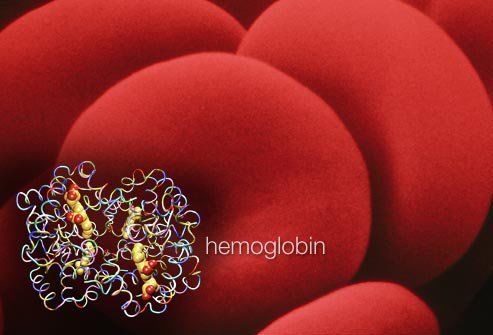
Anyone Can Have It
This illness means you have a lower than normal red blood cell (RBC) count. Normal values vary; blood tests like the complete blood count (CBC) can be explained by your doctor. Anemia may also result from low levels of hemoglobin, the protein that transports oxygen to the body. No matter what the cause, less oxygen is available and this produces weakness, dizziness, and shortness of breath. It is treatable once the underlying cause is identified. Long-standing or severe lack of oxygen can damage of the brain, heart, and other organs.
Causes
The three main causes of the illness are inadequate or faulty production of red blood cells, a high rate of destruction of red blood cells, and excessive bleeding. Megaloblastic anemia is one type of faulty red cell production. The condition of anemia has a wide range; it may be mild and easily treatable or severe and require immediate intervention.
Symptoms and Signs
Lack of Oxygen
The symptoms of anemia may range from mild and minimal to severe and incapacitating, potentially even life-threatening. It may be difficult to carry out normal, everyday activities. With hypoxia, the heart has to work harder to support the body.
Symptoms and Signs
Anemia can affect many systems in the body and produce a variety of symptoms and signs that affect health including
dizziness,
weakness,
pallor,
headache,
cold hands and feet,
numbness, and
low body temperature.
Heart Symptoms

Workload of the Heart
When hypoxia is present, the heart has to work harder to deliver adequate oxygen to the body. This may contribute to several cardiac-related symptoms including shortness of breath, chest pain, low blood pressure, and arrhythmia. Receiving treatment can help alleviate cardiac-related symptoms.
Causes in Children

A Problem in Infancy
Low iron may develop as soon as within the first year of life. Babies who are born prematurely or who are exclusively breast fed or fed formula that does not contain adequate levels of the mineral are at risk. Babies between the ages of 1 and 2 years old may become anemic from a lack of intake of sufficient iron-rich foods in their diets or from drinking too much cow's milk, which reduces absorption of the mineral. Ensure that a child gets adequate nutrient intake.
Pica
People who are deficient in iron may experience an intense urge to eat strange things like ice, clay, dirt, or starch. This behavior is called pica. This is alarming as low levels of this mineral can significantly negatively affect the development of the brain so it is very important to diagnose and treat the iron deficiency disease early.
Risk Factors

Who Gets Anemia?
Anyone of any age, race, and gender can develop the disorder. Menstruating women are most likely to suffer from it due to monthly blood loss. It may also occur during pregnancy if nutrient levels get too low. Blood volume increases during pregnancy but plasma expands more quickly than red blood cells are able to proliferate. This results in insufficient quantities of red blood cells.
Other Risk Factors
Many other risk factors may contribute. Your body needs the building blocks to make adequate red blood. Insufficient levels of certain nutrients may contribute. Bleeding due to injury or surgery are potential causes. Medical issues like chronic infections and disease states including cancer, ulcerative colitis, rheumatoid arthritis, kidney disease, liver disease, thyroid disease, heart failure, inflammatory bowel disease, and HIV/AIDS may play a role. Finally, there are certain inherited types of disease that result in low amounts of red blood cells (see following slides).
Teens

Both male and female teens may be at risk for anemia due to growth spurts. If a teen is experiencing fatigue, a health screening for iron-deficiency and other diseases is warranted. Severe low iron may predispose a teen to a higher risk of injuries and certain infections. If a severe lack exists, a doctor may recommend avoiding contact sports. Heavy menstrual periods, prior history, and low iron intake may contribute.
Low Iron Intake

A Critical Mineral
Iron is an essential component of hemoglobin, the protein that carries oxygen. The mineral is found both in plant foods and animal foods. It is better absorbed from animal sources. Factors and procedures that affect nutrient absorption in the gastrointestinal tract may impede absorption of necessary nutrients. Health factors like celiac disease, Crohn’s disease, and having undergone gastric bypass surgery may all negatively impact nutrient absorption.
Substances That Inhibit Mineral Absorption
Certain foods, supplements, and medications may inhibit the absorption of iron. The following substances should not be taken within several hours of taking the mineral - calcium-rich foods, dairy, tea, calcium supplements, coffee, and antacids.
Vitamin Deficiency

Necessary Nutrients
The body needs several essential vitamins and other nutrients to build red blood cells. Eating a diet that is low in iron, folate, B12, and protein may result in anemia. Conditions that impact absorption in the gastrointestinal tract may also contribute. The best way to ensure adequate intake of nutrients is to eat a varied, balanced diet. Diets that restrict certain food groups or diets that do not contain sufficient animal-based foods may increase the risk of anemia.
Good Sources of Iron
Lean meat and seafood are the best sources of the heme form of iron, the most bioavailable form of the mineral. Beans, vegetables, nuts, and fortified cereals are good sources of the nonheme form, which is less bioavailable. Poultry, meat, ascorbic acid, and seafood all help increase the absorption of the nonheme form. Compounds called phytates found in beans and grains inhibit absorption of the mineral. Certain polyphenols in cereals and legumes have a similar effect.
Some of the best food sources of the mineral from greatest to least include fortified breakfast cereal, oysters, white beans, chocolate, beef liver, lentils, spinach, and tofu.
Anemia of Chronic Disease

Chronic Illness and Infection
In addition to dietary factors, chronic illness and infection may lead to anemia by decreasing the amount of red blood cells that the body makes. This results in a small drop in hemoglobin levels. Health factors including cancer, inflammatory bowel disease, kidney disease, and rheumatoid arthritis are just a few illnesses that may lead to the disorder. In these instances, inflammatory molecules affect the way iron is stored and utilized in the body and less is available to make red blood cells.
Treatment
Improve your health by identifying and treating the underlying cause of maladies. Even mild cases of anemia of chronic disease may contribute to an increased risk of mortality and hospitalization in elderly people. For these reasons, it is very important to diagnose and treat the disorder, regardless of the cause. When treating the underlying cause is not always enough to resolve the issue, supplements may be prescribed. Oral and intravenous forms are available. It is possible to have an allergy to the IV form. Sometimes erythropoiesis-stimulating agents (ESAs) may be used to encourage the formation of more red blood cells.
Aplastic Anemia
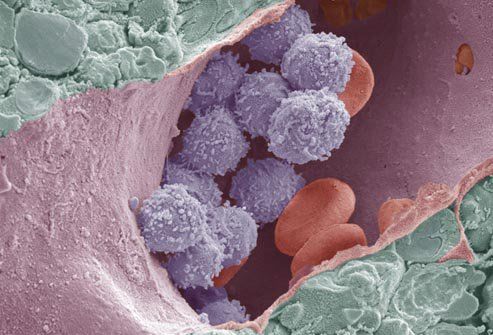
This illness results when the bone marrow makes insufficient blood for the body. The condition results in lower than expected levels of RBCs, white blood cells (WBCs), and platelets. It may either be inherited or acquired. Acquired cases may come on suddenly or develop slowly. There are several potential underlying causes of the acquired form including toxins, infectious diseases, autoimmune disorders, radiation, chemotherapy, and pregnancy. Myelodysplastic syndrome is a related illness.
Treatment
Effective treatment consists of certain medications, transfusions, or bone marrow stem cell transplants. Medications work by a variety of mechanisms. Some may stimulate the production of more blood. Medications in this class include erythropoietin and colony-stimulating factor. Medications that suppress the immune system, including cyclosporine, methylprednisolone, and anti-thymocyte globulin (ATG), may be prescribed. A low WBC count may increase the risk of infections, so the doctor may prescribe antiviral or antibiotic medications to decrease this risk.
Bleeding

Normal Causes
Bleeding decreases the number of RBCs in the body. Heavy menstruation, or menorrhagia, may cause this. Teens may be prone to this problem and should be screened annually, or more frequently if problems arise.
Other Causes
Ulcers in the gastrointestinal tract, internal or external injury, and surgery may also cause bleeding to a degree sufficient to lead to iron-deficiency anemia. In severe cases, a transfusion may be necessary to replace what was lost.
RBC Destruction

Inherited Illnesses
Certain inherited illnesses may cause an abnormally high destruction of RBCs. Sickle cell illness, thalassemias, and certain conditions associated with a lack of enzymes are a few types of inherited illnesses. These lead to the creation of defective RBCs that die faster than healthy RBCs.
Hemolytic Anemia
This is another illness that leads to the destruction of RBCs. It may be acquired or inherited. The acquired form may occur due to autoimmune illness, infections, tumors, leukemia, or lymphoma. It may also be a side effect of certain medications, including some types of antibiotics, anti-seizure medications, medications used to treat urinary tract infections, and others. These medications sometimes trigger the immune system to make antibodies against RBCs, which leads to their destruction.
Sickle Cell Disease

Inherited Illness
This is a group of several inherited disorders that affect the shape and function of RBCs. People with it have abnormal hemoglobin protein, called hemoglobin S, in their RBCs. This can decrease oxygen levels. The RBCs of someone who has it take on a characteristic sickle shape. They burst easily. It is a lifelong condition and the impact on health varies from person to person. The only cure is a marrow transplant but researchers are developing other treatments. A compatible donor is required for this technique to have the greatest chance of potential success. The illness is most common in people of Hispanic or African American descent.
Sickle Cell Anemia
Normal RBCs have a lifespan between 90 and 120 days. RBCs in someone with this illness live for between 10 to 20 days. The body may struggle to continuously manufacture new RBCs and the patient may feel fatigued. Crisis occurs when tissues and organs fail to receive adequate oxygen resulting in pain. Long term lack of oxygen may damage the joints, bones, spleen, lungs, liver, brain, lungs, eyes, skin, and other tissues.
Diagnosis

Complete Blood Count
A CBC, is often the first test that is ordered to confirm or rule out many illnesses. This test measures the level of hemoglobin in RBCs. It measures hematocrit, which is a ratio of the volume of RBCs compared to the total blood volume. The test also measures the levels of RBCs, WBCs, and platelets. Abnormal values of these may help diagnose an illness. Normal levels of these values may differ somewhat according to ethnic heritage. Another measure that may be assessed with a CBC is mean corpuscular volume (MCV). This measure determines the average size of RBCs.
Family History and Physical
In addition to a CBC, the doctor will take a complete personal and family health history and perform an exam to determine the status of a patient. The doctor will listen to your heart and lungs to assess heart rate and breathing. The doctor may check the size of the liver and spleen and assess for any tenderness.
Other Tests

Blood Tests
There are other tests that may be performed. Hemoglobin electrophoresis detects the different types of hemoglobin that are present. A reticulocyte count assesses how well and how quickly RBCs are manufactured. Serum iron, serum ferritin, total iron-binding capacity, and transferrin level are tests that assess different measures of iron status.
Bone Marrow Tests
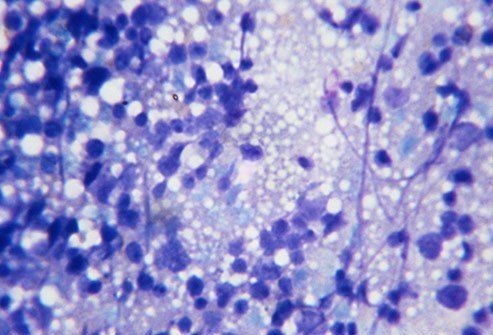
Needle Aspiration
If tests show marked abnormalities, a doctor may order an exam of the spongy material in the middle of long bones, which manufactures blood. A needle aspiration involves removing a small amount of tissue from the center of a bone (usually a hip) with a thin needle. The tissue is sent to the pathology lab for analysis. This test may help determine the cause of both high or low counts.
Needle Biopsy
A needle biopsy is similar to a needle aspiration in that it involves the insertion of a needle into the posterior iliac crest (back of the hipbone) to extract bone marrow for analysis. It differs from needle aspiration in that a larger needle is used to extract a larger amount of tissue from the hip. The test may be associated with some pain and discomfort. The doctor can administer anesthetic and a sedative to make the procedure as tolerable as possible.
Normal RBC Ranges
Levels Differ
Normal RBC ranges are different for men and women. The values are adjusted for altitude. The values are different because men, in general, have larger bodies than women. Men have larger blood volumes than women. The normal RBC value for men is 5 to 6 million cells/microliter. The normal range for RBCs in women is 4 to 5 million cells/microliter.
Treatment

Supplements
Mild to moderate iron deficiency may be treated with a variety of dietary changes and supplements. Ferrous is a form that is more easily absorbed than ferric. The mineral is best absorbed when taken with a meal and along with vitamin C. Orange juice is a good thing to consume along with the supplement to aid absorption. Folic acid and vitamin B12 are also necessary to manufacture healthy RBCs. The doctor may recommend eating a diet rich in folate and vitamin B12 or supplementing these necessary nutrients.
Blockers
Some substances in certain foods, beverages, and supplements may interfere with the ability to absorb enough iron. Calcium blocks the absorption of the mineral. If you take calcium, ask the doctor how many hours you should take it away from other supplements you take. Do not take supplements with coffee or tea. These beverages contain substances that may inhibit absorption.
Iron-Deficiency Anemia and Pregnancy

Requirements in Pregnant Women
A woman’s blood volume increases by approximately 20% to 30% during pregnancy. This increases her requirements for nutrients to make enough red blood. Approximately half of pregnant women develop deficiency during pregnancy. Pregnant women should aim to get enough iron (27 milligrams) in their diets every day to ensure adequate iron levels. The doctor will perform regular health check-ups on pregnant women. Prenatal vitamins contain necessary minerals to help prevent deficiency.
After Delivery
Women may hemorrhage during or after delivery. If severe loss has occurred, a transfusion may be necessary to protect her health. Potential side effects of a transfusion may include a headache, rash, itching, and fever.
Medication Treatment

Treat the Underlying Cause
Successful treatment involves identifying and treating the underlying cause. If a bacterial infection is to blame, antibiotics may resolve the infection. If heavy menstrual bleeding is the reason, hormones may be prescribed to mitigate blood loss. Erythropoietin (EPO) is a hormone that can stimulate the production of red blood cells. Corticosteroids may be prescribed to block immune system destruction of red blood cells. Hydroxyurea is a cancer drug that may be used. Every medication is associated with potential risks and benefits that must be weighed for each indication and each patient.
Chelation
Chelation is a procedure that involves the use of a chelating agent, ethylene diamine tetra-acetic acid (EDTA), to remove lead, mercury, and other heavy metals from the body. The procedure is used mostly in children. Kids who have iron-deficiency anemia are at increased risk of lead poisoning.
Transfusion

Treatment for Severe Conditions
In the event of severe deficiency and/or if there has been a lot of blood loss, a transfusion may be necessary. Blood loss may occur during surgery, due to an injury, or during or after childbirth. The recipient’s blood is “typed” prior to transfusion to ensure a compatible blood type is used. In the event of an emergency, universal donor blood is transfused into the patient. Blood is transfused via an IV and it takes between 1 and 4 hours.
Bone Marrow Transplant
Certain types of cancer, aplastic anemia, and illnesses that interfere with RBC production may be treated with a bone marrow transplant. This involves receiving either autologous (derived from the self) or allogenic (from a compatible donor) stem cells to restore production of healthy blood. Before being infused with the new tissue, the recipient receives chemotherapy, radiation, or both to destroy the existing tissue. The new system can then begin producing new, healthy blood.
Prevention

Dietary Strategies
Eating a healthy, balanced diet may help prevent deficiencies. Give your body all of the necessary building blocks to produce healthy blood. Liver, red meat, beans, lentils, tofu, fish, dried fruit, and dark leafy greens are good. Vitamin B12 and folic acid are necessary for the production of RBCs, too. Dairy products, eggs, bananas, and spinach are rich in these. Fortified breads, cereals, and pastas contain necessary minerals, vitamin B12, and folic acid. Citrus fruits and other forms of produce are high in vitamin C, which is also necessary.
Treat the Underlying Cause
Treating the underlying cause of a deficiency may help prevent future bouts. If a medication is contributing, ask the doctor about switching to something else that does not have unwanted side effects. Many conditions may have an effect on the blood. Treating and controlling the primary disease may help prevent future bouts of deficiency.
Hemochromatosis
Too Much of a Good Thing
Just as deficiency can cause problems, so can too much iron or hemochromatosis. It is a genetic condition that causes increased absorption of the mineral in the body. Toxic levels build up and can damage organs, especially the liver and kidney. Most cases of hemochromatosis are inherited, but some are acquired. Approximately half of all people who have the genetics for hemochromatosis do not exhibit characteristic problems of the disease.
Hemochromatosis Treatment
Treatment for hemochromatosis begins with minimizing the absorption of iron by making dietary changes. Avoid taking supplements and limit intake of vitamin C, which increases the absorption of the mineral. Is it recommended to avoid raw fish and shellfish when one has hemochromatosis to minimize the risk of acquiring a bacterial infection. Therapeutic phlebotomy is a procedure similar to blood donation that helps lower excess stores of the mineral. Chelation involves taking a chelating agent by mouth or via IV to bind and remove excess minerals.
Living With Anemia

Manage It
It is possible to live well with your diagnosis. Eating a varied, balanced diet is one way to keep nutrient stores and energy levels up. Many people who have deficiency can keep symptoms at bay by eating sufficient iron, vitamin B12, and folic acid, or by supplementing these necessary nutrients.
Get to the Root Cause
If an underlying illness is responsible for your symptoms, treating and managing the underlying condition should help keep anemia symptoms at bay. Cancer, kidney disease, ulcerative colitis, rheumatoid arthritis, or other illnesses may be to blame. Work with your doctor to determine the underlying cause and treat it to prevent future bouts of low iron.











