
Muscle Cramps (Charley Horse) and Muscle Spasms
Muscle Cramps vs. Muscle Spasms
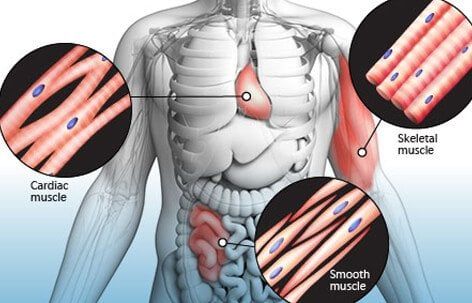
There are three types of muscles in your body. Cardiac muscle makes up your heart. Smooth muscle cells line your blood vessels, gastrointestinal tract, and certain organs. Skeletal muscles attach to your bones and are used for voluntary movements of the body. Muscle spasms occur when a skeletal muscle contracts and does not relax. Muscle spasms are forceful and involuntary. A sustained muscle spasm is called a muscle cramp. Leg muscles, especially the quadriceps (thigh), hamstrings (back of thigh), and gastrocnemius (calves), are most likely to cramp, but any skeletal muscle in the body can cramp. A "charley horse" is another name for a muscle cramp.
What Causes Muscle Cramps?

There are many potential causes of muscle cramps including physical exertion in hot weather, overexertion, dehydration, electrolyte imbalance, and physical deconditioning. Many times, muscle cramps are not cause for alarm; however, at other times muscle cramps may indicate a more serious underlying problem such as liver cirrhosis, atherosclerosis, ALS, thyroid disorders, or a problem or issue with the spine or spinal nerves. Certain medications and supplements may be associated with muscle cramps.
Signs and Symptoms of Muscle Cramps

Muscle cramps can range from being a mild nuisance to incapacitating and extremely painful. The cramped muscle may be visibly distorted or look knotted. Twitching may be evident. The area of a muscle cramp may be firm to the touch. Some muscle cramps last just a few seconds, while others can last 15 minutes or more.
Medications That Cause Muscle Cramps

High blood pressure medications, insulin, birth control pills, cholesterol-lowering medications, and certain types of asthma medications (beta-agonists) may cause muscle cramps. These medications cause cramps by a variety of mechanisms. They may interfere with electrolyte levels, contribute to the breakdown of muscle tissue, or interfere with blood flow. Report medication-related muscle cramps to your doctor.
Muscle Cramps at Night

Muscle cramps at night, especially in the calves, are very common and affect up to 60% of adults. Women are more likely to suffer from nocturnal leg cramps than men. They are also more common with age and contribute to insomnia. Muscle fatigue and nerve dysfunction are believed to contribute to nocturnal leg cramps. Management of nocturnal leg cramps may include stretching, massage, and treatment of any underlying disorders that contribute to the condition.
Muscle Cramps during Pregnancy

Many pregnant women experience muscle cramps, especially in the legs and at night. The levels of fluids and electrolytes in the body fluctuate during pregnancy, which may contribute to leg cramps. Increased pressure on pelvic nerves may also play a role.
Muscle Cramp Remedies and Treatment

The vast majority of leg cramps resolve on their own within a few minutes without treatment. As soon as a muscle cramp comes on, stop doing the activity that precipitated it. Stretching and massaging the area may help relieve muscle cramps. Apply heat to help relax a cramped muscle. A cold pack and nonsteroidal anti-inflammatory drugs (NSAIDs) help relieve pain. Always consult a doctor if muscle cramps are severe or if they recur frequently.
Medications to Treat Muscle Cramps

Pain medications, muscle relaxants, and anticonvulsants may be used to treat muscle cramps. It's best to use lifestyle interventions like hydration, stretching, and the application of heat and cold to treat muscle cramps, but medication may be helpful when other strategies are ineffective.
Muscle Symptoms and Anxiety
Generalized anxiety disorder (GAD) may include symptoms like muscle aches, muscle tension, and twitching. Anxiety is often accompanied by other body symptoms such as fatigue, sweating, nausea, and shortness of breath.
Muscle Cramp Prevention

Strategies for reducing the risk of muscle cramps include varying exercise routines, staying well hydrated, and stretching. Warm up by jogging or walking at a brisk pace before stretching the calves, hamstrings, and quads. Maintaining good levels of electrolytes will help, too. Sodium and potassium are lost during exercise, especially in the heat and with excessive sweating. Sports drinks can help replenish sodium and potassium.











